Delegates at our COVID Recovery webinar listened to how we are working with 80 areas to help accelerate their COVID-19 recovery. We’ve edited the discussion into a weekly 3 blog article series. If you missed Week 1 & 2 – the discussions can be found here:
5 minutes with our Referral Backlog Triage Lead
5 minutes with our Dermatology Lead
This week we are focussing on the use of Advice & Guidance. The discussion was between our CEO Jonathan Patrick, and Lucy Sammons, our Customer Success Lead.
What have we learnt from activity during COVID?
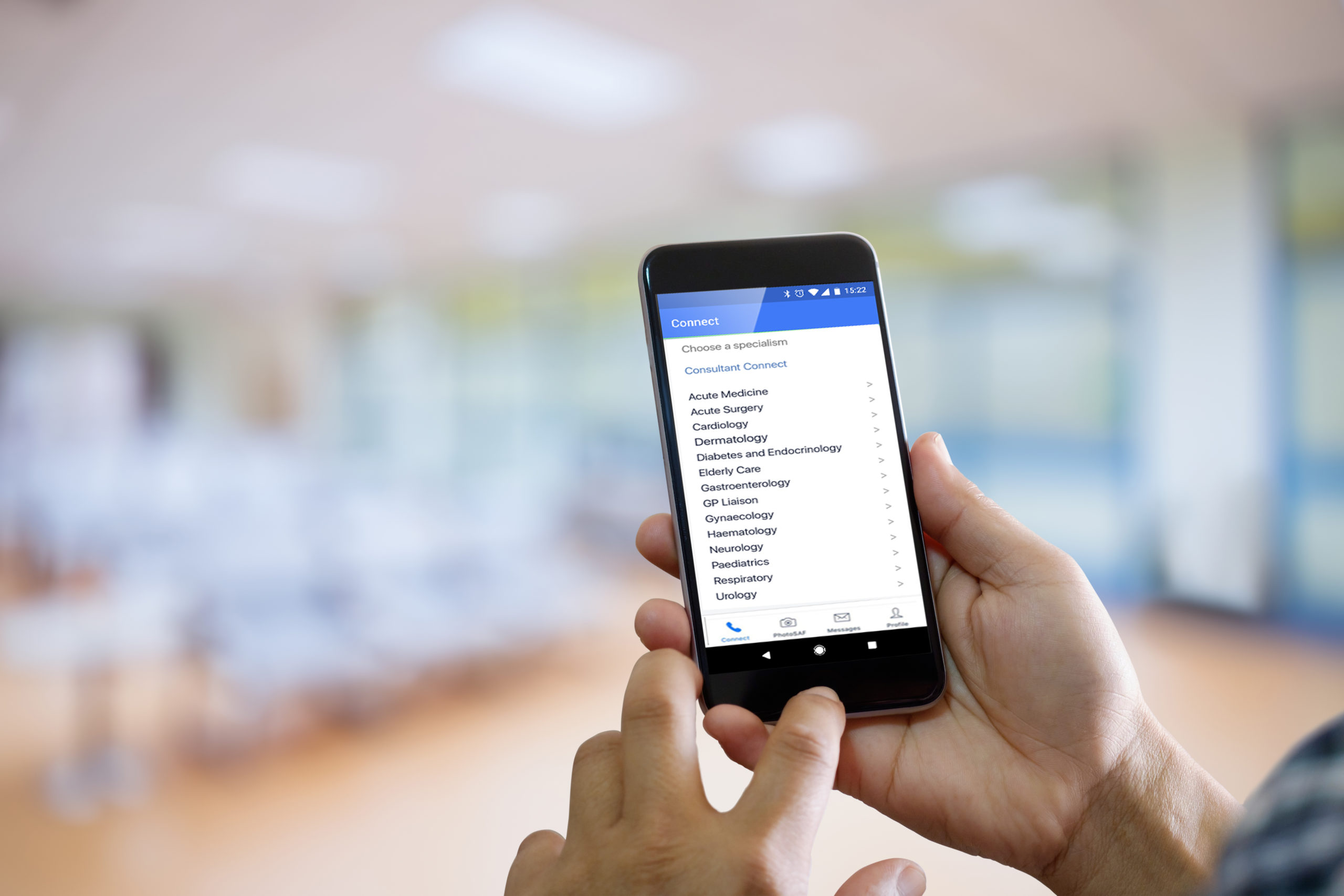
Generally, there’s been a more integrated and interconnected approach to advice and guidance, including making sure that Ambulance Trusts, Community Teams and Care Homes have rapid access to the right advice and guidance. Over the last year we’ve become much more multifaceted in the way we deliver and configure Consultant Connect projects which has been great to see.
During the pandemic we saw an expansion of specialty advice and guidance lines across both Primary Care and Community Care setting. Within that, dedicated COVID advice and guidance lines were added in over 40 of our projects and have proved really effective with over 8,000 calls taken to date.
Patient initiated follow-up was introduced at the very start of COVID to aid with patient discharge. Via our system, we enable patients to have a direct dial number back into the ward that they were discharged from. To complement this, we have a follow-up system that enables consultants, registrars, and nurses to call patients back remotely – helping to keep patients out of a hospital setting when appropriate.
We have also been supporting hot hubs by ensuring that they are set up to receive targeted COVID advice and guidance. All activity is tracked which enables us to be constantly agile and refine our services to best support the teams.
It’s been great to also support mental health teams, particularly enabling inpatient wards to get rapid physical advice and guidance. This has proven really effective in ensuring that patients remain in the right setting for physical treatment.
How can we support the recovery and the restoration of services in the NHS?
When it comes to recovery and restoration it’s about utilising data to inform action, looking at our data in combination with our client partner’s data and helping to shape the agile solutions. No two projects are the same, so we work really closely with our client partners to constantly refine how we provide operational support.
All project activity is tracked in the secure Consultant Connect dashboard, giving commissioners and hospitals a really good understanding of the pressure points and trends.
We are seeing an increased focus on managing patients with long-term conditions (LTCs). In order for Primary Care and Community Teams to be really well supported in the day-to-day management of patients with LTCs we are setting up more specialist advice lines e.g., direct to Diabetic Specialist Nurses, Heart Failure Nurses, and COPD Nurses.
The integration of Community Teams is playing an ever-important role in the shared care model. For example, providing Community Teams both with advice and guidance from Secondary Care, but also supporting Secondary Care teams via access to Community teams, in patient discharge – so being really joined up. And equally allowing Community Teams to have back up from Primary Care via bypass numbers. It is really about finding ways to continue to facilitate the ease of communication from one healthcare professional to another.
There’s also a real focus on frailty spanning Primary Care, Community Teams, Secondary Care teams, Ambulance Trusts, and Care Homes. We are making sure all of those teams are interconnected and that the pathways are clearly understood, so that there’s no risk of a patient ending up in the wrong setting.
Our Photo and Messaging advice and guidance service has also grown hugely over the past year enhancing both local and community pathways. It has proven really effective across many specialties including Ophthalmology (supporting Community Optometrists) and Dermatology, allowing many patients to remain in the community or Primary Care setting – when appropriate.
We’ve also started work, across the UK, on the ‘Phone First’ or ‘111 First’ initiatives being rolled out. Consultant Connect is really well placed as we are effectively the ‘communication plumbing’ between one healthcare professional and another!
Finally, I think enhanced and rapid cross-hospital communication will be critical to recovery and restoration. We have been supporting hospitals with their ‘Perfect Week’ initiatives this way, to aid patient flow and early discharge. Hospitals we work with are seeing the immediate benefits of connecting teams (e.g. therapies, radiology, pharmacy, and junior colleagues with their more senior peers etc).
Related links