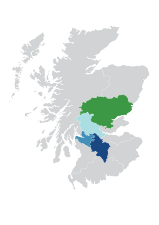
Consultant Connect in NHS Scotland
Professional-to-Professional clinical decisions
Primary Care clinicians refer fewer patients to hospital if they get timely specialist input first. Our services enable them to access Professional-to-Professional clinical decisions (Prof-to-Prof) to safely manage more patients in the community.
What are the benefits of Prof-to-Prof?
- Connects rural communities, enhancing communication between healthcare professionals
- All data is stored in the cloud, making the service IG-secure so it can be used with complete confidence on personal devices
- Users can be attached to multiple organisations (in participating NHS areas), which is ideal for locum clinicians
- Activity is recorded and tracked for medico-legal purposes, and can be used to inform decisions within teams and provides a valuable training tool
- Helps prevent unnecessary hospital conveyances, ensuring patients get the right care in the right place the first time

See what your colleagues say

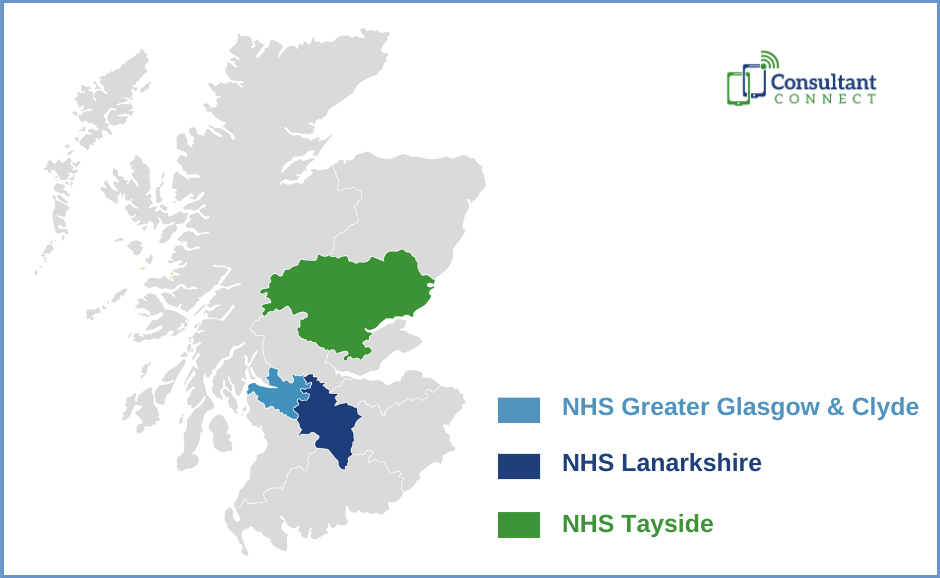
Urgent Prof-to-Prof Radiology Advice helps speed up prostate cancer diagnosis

The Acute Paediatrics line that has tripled Consultant Connect usage in NHS Lanarkshire

How the Infectious Diseases Advice line in Greater Glasgow and Clyde is speeding up clinical communication

5 minutes with… the Flow Navigation Centre clinicians in NHS Lanarkshire

Paediatrics Professional-to-Professional Advice speeds up patient care in Greater Glasgow and Clyde Health Board

GP case study: Mental Health advice in Greater Glasgow and Clyde

5 minutes with… a Lead Nurse

Area Case Study | COPD Pathway in NHS Tayside

Area Case Study | Patient Connect in NHS Lanarkshire

NHS Lanarkshire Prof-to-Prof Advice GP case study
Consultant Connect in NHS Scotland
Services and Impact in NHS Scotland
Find out how Scottish Health Boards and the Scottish Ambulance Service are using Consultant Connect to transform communication and improve patient care.
Best Practice Guidance for Professional to Professional Decision Support
Consultant Connect in NHS Scotland
Services and Impact in NHS Scotland
Find out how Scottish Health Boards and the Scottish Ambulance Service are using Consultant Connect to transform communication and improve patient care.
Best Practice Guidance for Professional to Professional Decision Support
Contact Us

Consultant Connect services
supporting NHS areas across the UK
Referral Triage and Validation
Our clinically-led Referral Triage and Validation service supports hospitals needing additional temporary capacity for referrals. The service uses the clinical expertise of NHS consultant, across 17 specialties from our National Consultant Network (NCN). Working remotely, as ‘virtual locums’ they follow local pathways and protocols, and, under the leadership of local clinical leads, support with triaging and validating waiting list backlogs in bulk or and/or new referrals as they come in. On average 29% of referrals reviewed through the service are taken off the waiting list and patients returned to their GP with management plans.

National Consultant Network
The National Consultant Network (NCN) comprises out-of-area NHS consultants who can answer pre-referral Prof-to-Prof calls or review photos and messages. The consultants can act as a backup for local teams and provide locally unavailable specialties. If you are short of staff, the NCN can be switched on in just 24-48 hours. It can also be switched off that quickly when it’s no longer needed.

Patient Connect
Clinicians use Patient Connect to deliver IG-secure virtual consultations, allowing them to contribute to patient care whilst working remotely. Patients receive the right care faster, and clinicians only see the patients they need to see. All data and call recordings are available via Consultant Connect in your browser.

Patient Initiated Follow Up
Our Patient Initiated Follow Up Service (PIFU) service enables patients to initiate an IG-secure virtual consultation with a specialist clinician.
The service reduces unnecessary visits to hospital, patient waiting times and releases the clinical teams to see patients in a more timely manner.
There is no doubt that this is the simplest, most effective way of delivering follow-up consultations where the clinician does not need to see the patient.

Telemedicine Devices
Our state-of-the-art virtual care devices allow NHS specialists to be fully available in the care of patients, without having to be physically at the bed side. The devices are easily replicable across a number of settings, whether it is instant access to Prof-to-Prof, to help with resuscitation, or for routine ward rounds, the timely delivery of safe care is a key factor. As well as providing remote support and reassurance to colleagues, the devices help make job planning far more efficient with the reduction in cross-site travel, enabling self-isolating or shielding consultants to participate and a reduction in locum costs.
Referral Triage and Validation
Our clinically-led Referral Triage and Validation service supports hospitals needing additional temporary capacity for referrals. The service uses the clinical expertise of NHS consultant, across 17 specialties from our National Consultant Network (NCN). Working remotely, as ‘virtual locums’ they follow local pathways and protocols, and, under the leadership of local clinical leads, support with triaging and validating waiting list backlogs in bulk or and/or new referrals as they come in. On average 29% of referrals reviewed through the service are taken off the waiting list and patients returned to their GP with management plans.

National Consultant Network
The National Consultant Network (NCN) comprises out-of-area NHS consultants who can answer pre-referral Prof-to-Prof calls or review photos and messages. The consultants can act as a backup for local teams and provide locally unavailable specialties. If you are short of staff, the NCN can be switched on in just 24-48 hours. It can also be switched off that quickly when it’s no longer needed.

Patient Connect
Clinicians use Patient Connect to deliver IG-secure virtual consultations, allowing them to contribute to patient care whilst working remotely. Patients receive the right care faster, and clinicians only see the patients they need to see. All data and call recordings are available via Consultant Connect in your browser.

Patient Initiated Follow Up
Our Patient Initiated Follow Up Service (PIFU) service enables patients to initiate an IG-secure virtual consultation with a specialist clinician.
The service reduces unnecessary visits to hospital, patient waiting times and releases the clinical teams to see patients in a more timely manner.
There is no doubt that this is the simplest, most effective way of delivering follow-up consultations where the clinician does not need to see the patient.

Telemedicine Devices
Our state-of-the-art virtual care devices allow NHS specialists to be fully available in the care of patients, without having to be physically at the bed side. The devices are easily replicable across a number of settings, whether it is instant access to Prof-to-Prof, to help with resuscitation, or for routine ward rounds, the timely delivery of safe care is a key factor. As well as providing remote support and reassurance to colleagues, the devices help make job planning far more efficient with the reduction in cross-site travel, enabling self-isolating or shielding consultants to participate and a reduction in locum costs.
Contact us
For more information about how we work with commissioners, hospitals and mental health trusts to improve patient care, please get in touch.
Join a webinar
Listen to health experts from the comfort of your desk as we bring the experts to you in our series of online webinars.
Join our mailing list
Join our mailing list and we'll keep you informed of our latest blogs, project news, and upcoming webinar dates and topics.