‘Virtual locum’ NHS consultant capacity available
Did you know our network of remote NHS consultants can deliver Advice & Guidance on local referral systems (e.g., e-RS) plus triage and validate referrals, reducing waiting lists by a third on average?
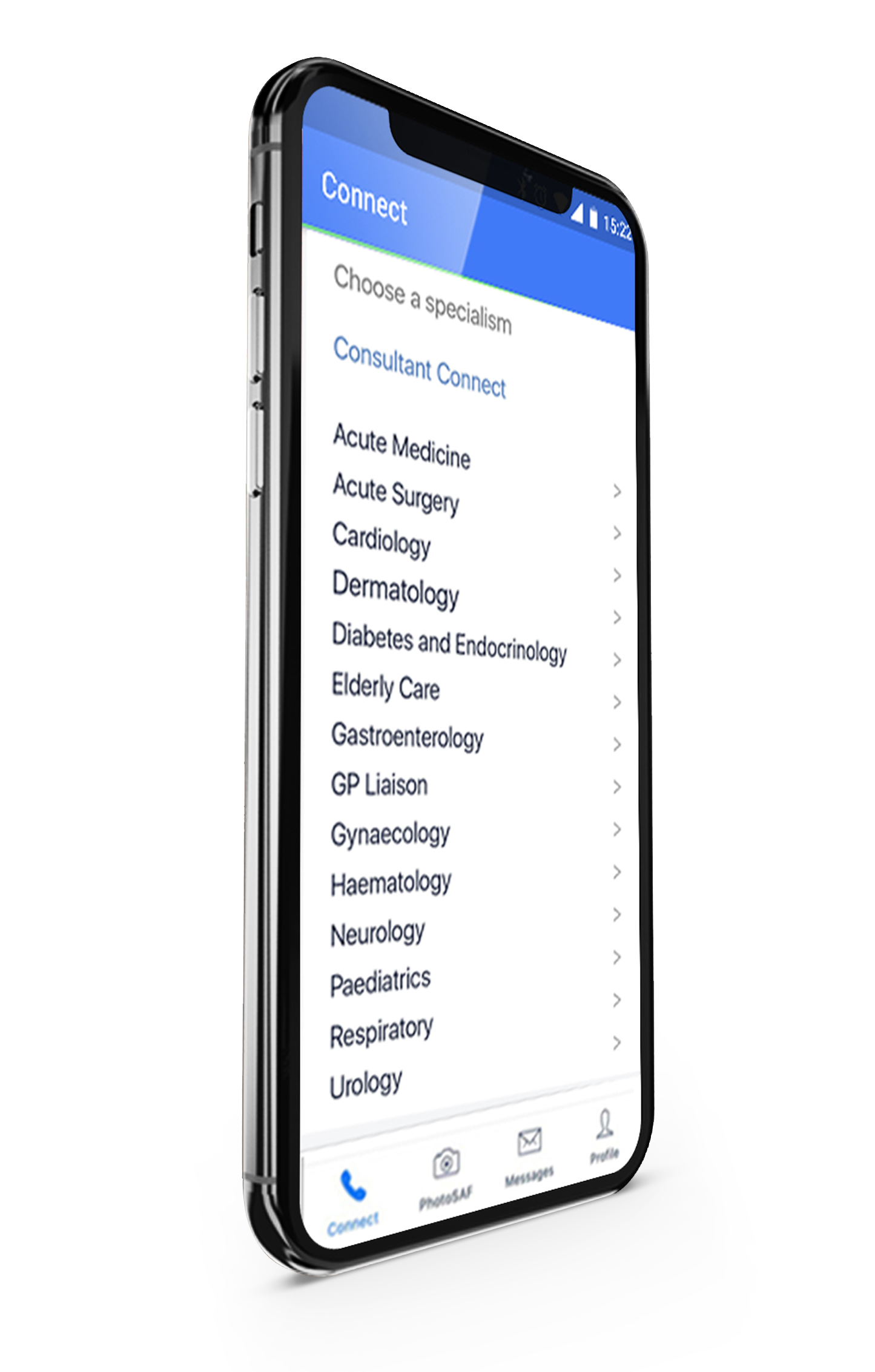
Enhanced Advice & Guidance
Supported by the National Consultant Network, our Enhanced Advice & Guidance service consists of Telephone Advice & Guidance, Photo Messaging Advice & Guidance, and Email Advice & Guidance, as well as Referral Triage and Validation for areas with high backlogs.
Advice and Refer
Advice and Refer by Consultant Connect links our Enhanced A&G platform, which is already used by over half the NHS, with the e-RS referrals system. It is the easiest, most seamless way to review a patient’s case and, if necessary, refer that patient to a local clinic.
National Consultant Network (NCN)
The National Consultant Network comprises out-of-area NHS consultants who can answer pre-referral Advice & Guidance calls or review photos and messages. The consultants can act as a backup for local teams and provide locally unavailable specialties.
Referral Triage and Validation
NHS consultant capacity to triage backlogs and temporarily support with restoration of services.
Telemedicine Devices
State-of-the-art virtual care devices allow NHS specialists to be fully available in the care of patients, without having to be physically at the bed side.
Patient-Initiated Follow-Up (PIFU)
A follow-up service that enables patients to initiate an IG-secure virtual consultation with a specialist clinician. All data and call recordings are available via Consultant Connect in your browser.
Virtual Consultations (Patient Connect)
Clinicians use Patient Connect to deliver IG-secure virtual consultations. All data and call recordings are available via Consultant Connect in your browser.
Enhanced Advice & Guidance
Supported by the National Consultant Network, our Enhanced Advice & Guidance service consists of Telephone Advice & Guidance, Photo Messaging Advice & Guidance, and Email Advice & Guidance as well as Referral Triage and Validation for areas with high backlogs.

Advice and Refer
Advice and Refer by Consultant Connect links our Enhanced A&G platform, which is already used by over half the NHS, with the e-RS referrals system. It is the easiest, most seamless way to review a patient’s case and, if necessary, refer that patient to a local clinic.
National Consultant Network (NCN)
The National Consultant Network comprises out-of-area NHS consultants who can answer pre-referral Advice & Guidance calls or review photos and messages. The consultants can act as a backup for local teams and provide locally unavailable specialties.

Referral Triage and Validation
NHS consultant capacity to triage backlogs and temporarily support with restoration of services.

Telemedicine Devices
State-of-the-art virtual care devices allow NHS specialists to be fully available in the care of patients, without having to be physically at the bed side.

Patient Initiated Follow up (PIFU)
A follow-up service that enables patients to initiate an IG-secure virtual consultation with a specialist clinician. All data and call recordings are available via Consultant Connect in your browser.

Virtual consultations (Patient Connect)
Clinicians use Patient Connect to deliver IG-secure virtual consultations. All data and call recordings are available via Consultant Connect in your browser.
Covering >40 million patients across over half the NHS in England, Scotland and Wales.
What we do
NHS commissioners explain why they like our services…
Consultant Connect
Consultant Connect is a telemedicine provider transforming patient care in the NHS through better communications.
By having immediate and direct access to specialist advice, clinicians can ensure that patients get the right care the first time. As this often means that patients avoid unnecessary trips to hospital, the NHS saves money and hospital specialists spend their time dealing with patients that they need to see. It’s a great outcome for everyone.
Read our case studies and blog to find out more!
Consultant Connect
Consultant Connect is a telemedicine provider transforming patient care in the NHS through better communications.
By having immediate and direct access to specialist advice, clinicians can ensure that patients get the right care the first time. As this often means that patients avoid unnecessary trips to hospital, the NHS saves money and hospital specialists spend their time dealing with patients that they need to see. It’s a great outcome for everyone.
Read our case studies and blog to find out more!
Contact us
For more information about how we work with commissioners, hospitals and mental health trusts to improve patient care, please get in touch.
Join a webinar
Listen to health experts from the comfort of your desk as we bring the experts to you in our series of online webinars.
Join our mailing list
Join our mailing list and we'll keep you informed of our latest blogs, project news, and upcoming webinar dates and topics.